Have you ever experienced "butterflies" in your stomach before an important presentation? Or felt that unexplainable "gut feeling" when making a decision? These common expressions aren't merely figures of speech - they reflect a profound scientific reality that researchers have been increasingly fascinated by: our gut functions as a second brain.
The Enteric Nervous System: Your Hidden Neural Network
Nestled within the walls of our digestive tract lies an intricate network of neurons called the enteric nervous system (ENS). This remarkable system contains over 500 million neurons—more than you'd find in your spinal cord (1). The ENS can operate independently from the central nervous system, making decisions about digestion, detecting potential dangers from ingested foods, and regulating gut motility without direct input from the brain. This autonomy is precisely why scientists have dubbed the gut our "second brain."
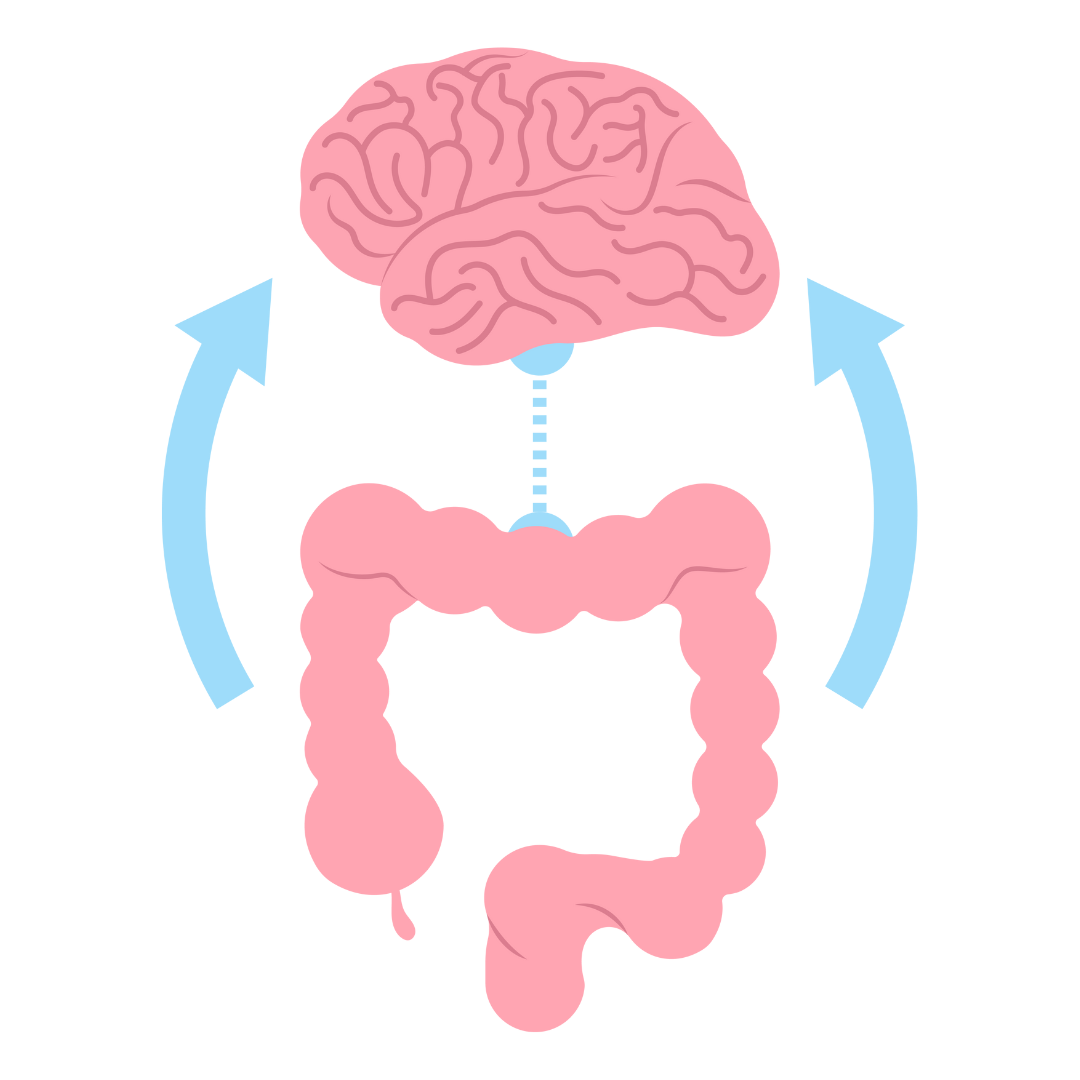
The Gut-Brain Axis: A Two-Way Communication Highway
The connection between our gut and brain operates via a complex communication system known as the gut-brain axis. This bidirectional highway includes neural pathways like the vagus nerve, immune system signalling, hormone regulation, and the production of neurotransmitters. Remarkably, about 95% of serotonin—our "happiness hormone"—is produced in the gut, not the brain (2). This explains why digestive issues often coincide with mood disorders like anxiety and depression.
Microbiome: The Tiny Residents With Enormous Influence
Within our digestive system resides a vast community of microorganisms collectively known as the gut microbiome. This ecosystem comprises trillions of bacteria, fungi, viruses, and other microbes that play crucial roles in our overall health. These microscopic residents help digest food, produce essential vitamins, protect against pathogens, and—most fascinatingly—influence our brain function and behaviour.
Research has shown that the composition of our gut microbiome affects everything from stress response and anxiety levels to cognitive function and social behaviour (3). Groundbreaking studies have even demonstrated that transferring gut bacteria from anxious mice to calm ones can induce anxiety-like behaviours in the previously calm mice—powerful evidence of the microbiome's influence on our mental state (4).
Gut Health and Mental Wellbeing: The Emerging Science
The connection between gut health and mental wellbeing has spawned a new field of research called "psychobiotics"—the study of how specific microorganisms can benefit mental health (5). Emerging evidence suggests that certain probiotic strains might help alleviate symptoms of depression, anxiety, and stress. This revolutionary approach offers a complementary pathway to traditional mental health treatments.
Stress and Your Second Brain: A Vicious Cycle
The relationship between stress and gut health exemplifies the intricate connection between our two brains. When we experience psychological stress, our central nervous system triggers changes in gut function—altering motility, increasing sensitivity, and disrupting the microbiome balance. Conversely, an unhealthy gut can send signals to the brain that heighten stress perception, creating a difficult cycle to break.
This explains why irritable bowel syndrome (IBS) and other functional gastrointestinal disorders often worsen during stressful periods (6). It's not merely a coincidence—it's a direct manifestation of the gut-brain communication system in action.
Inflammation: The Common Enemy
Chronic inflammation represents a shared mechanism through which poor gut health affects brain function. When the gut barrier becomes compromised—a condition often referred to as "leaky gut"—it allows bacterial components and inflammatory molecules to enter the bloodstream, triggering a systemic inflammatory response that can reach the brain (7). This neuroinflammation has been linked to mood disorders, cognitive decline, and even neurodegenerative conditions like Parkinson's disease.
Nutrition's Dual Impact
The foods we consume affect both our central and enteric nervous systems. A diet rich in processed foods, refined sugars, and unhealthy fats promotes inflammation and disrupts microbial balance. Conversely, a diverse, plant-based diet nourishes beneficial gut bacteria and provides the nutrients necessary for neurotransmitter production.
Particularly beneficial are fermented foods like yoghurt, kefir, and sauerkraut, which contain live beneficial bacteria; prebiotic fibre-rich foods like garlic, onions, and asparagus, which feed beneficial gut bacteria; and anti-inflammatory omega-3 fatty acids found in oily fish and flaxseeds.
Sleep, Exercise, and Your Second Brain
Both sleep and physical activity profoundly influence the gut-brain connection. Poor sleep quality disrupts the gut microbiome, while regular exercise enhances microbial diversity and strengthens the gut barrier (8). These lifestyle factors create another dimension in the complex relationship between our two brains, highlighting the importance of a holistic approach to health.
How JUVIA Supports Your Gut as a Second Brain
When it comes to nurturing the vital connection between your gut and brain, JUVIA offers a revolutionary approach with its unique ERME™ (Enzyme Rich Malt Extract) formulation. Unlike traditional probiotics that introduce foreign bacteria to your system, JUVIA works harmoniously with your body's native gut ecosystem, fostering the growth and diversity of beneficial bacteria whilst reducing harmful inflammation. This scientifically-backed solution contains over 15 natural enzymes that survive stomach acid—a significant advantage over conventional digestive enzyme tablets. By rebalancing your unique gut microbiome, JUVIA not only helps improve digestion and reduce bloating but also supports the critical gut-brain axis communication system. The enhanced nutrient absorption that JUVIA facilitates contributes to increased energy levels, whilst its positive impact on the gut microbiome may support better mood regulation and mental wellbeing. For those seeking to support both their digestive health and cognitive function through natural means, JUVIA represents a holistic approach firmly grounded in the emerging science of our second brain.
Nurturing Your Second Brain
Caring for your second brain is essential for overall wellbeing. This includes maintaining a diverse diet rich in fibre, limiting antibiotics when possible, managing stress through mindfulness and relaxation techniques, prioritising quality sleep, and engaging in regular physical activity. These practices not only support digestive health but potentially enhance mental clarity, emotional resilience, and cognitive function.
The discovery of our gut as a second brain represents one of the most exciting frontiers in medical science. As we continue to unravel the mysteries of the gut-brain axis, we gain deeper insights into the interconnected nature of our bodily systems and the profound ways they shape our physical and mental experiences. By honouring and nurturing this connection, we open pathways to more holistic health and enhanced quality of life—a testament to the remarkable wisdom encoded within our biology.
References
- Schneider, S., Wright, C. M., & Heuckeroth, R. O. (2019). Unexpected Roles for the Second Brain: Enteric Nervous System as Master Regulator of Bowel Function. Annual review of physiology, 81, 235–259. https://doi.org/10.1146/annurev-physiol-021317-121515
- Appleton J. (2018). The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integrative medicine (Encinitas, Calif.), 17(4), 28–32. https://pmc.ncbi.nlm.nih.gov/articles/PMC6469458/
- Kumar, A., Pramanik, J., Goyal, N., Chauhan, D., Sivamaruthi, B. S., Prajapati, B. G., & Chaiyasut, C. (2023). Gut Microbiota in Anxiety and Depression: Unveiling the Relationships and Management Options. Pharmaceuticals (Basel, Switzerland), 16(4), 565. https://doi.org/10.3390/ph16040565
- Luo, Y., Zeng, B., Zeng, L., Du, X., Li, B., Huo, R., Liu, L., Wang, H., Dong, M., Pan, J., Zheng, P., Zhou, C., Wei, H., & Xie, P. (2018). Gut microbiota regulates mouse behaviors through glucocorticoid receptor pathway genes in the hippocampus. Translational psychiatry, 8(1), 187. https://doi.org/10.1038/s41398-018-0240-5
- Lyte, M., & Cryan, F. (2014). Microbial Endocrinology: The Microbiota-Gut-Brain Axis in Health and Disease. Advances in Experimental Medicine and Biology, 817. https://www.researchgate.net/publication/321572287_Microbial_Endocrinology_The_Microbiota-Gut-Brain_Axis_in_Health_and_Disease
- Qin, H. Y., Cheng, C. W., Tang, X. D., & Bian, Z. X. (2014). Impact of psychological stress on irritable bowel syndrome. World journal of gastroenterology, 20(39), 14126–14131. https://doi.org/10.3748/wjg.v20.i39.14126
- Di Vincenzo, F., Del Gaudio, A., Petito, V., Lopetuso, L. R., & Scaldaferri, F. (2024). Gut microbiota, intestinal permeability, and systemic inflammation: a narrative review. Internal and emergency medicine, 19(2), 275–293. https://doi.org/10.1007/s11739-023-03374-w
- Dalton, A., Mermier, C., & Zuhl, M. (2019). Exercise influence on the microbiome-gut-brain axis. Gut microbes, 10(5), 555–568. https://doi.org/10.1080/19490976.2018.1562268