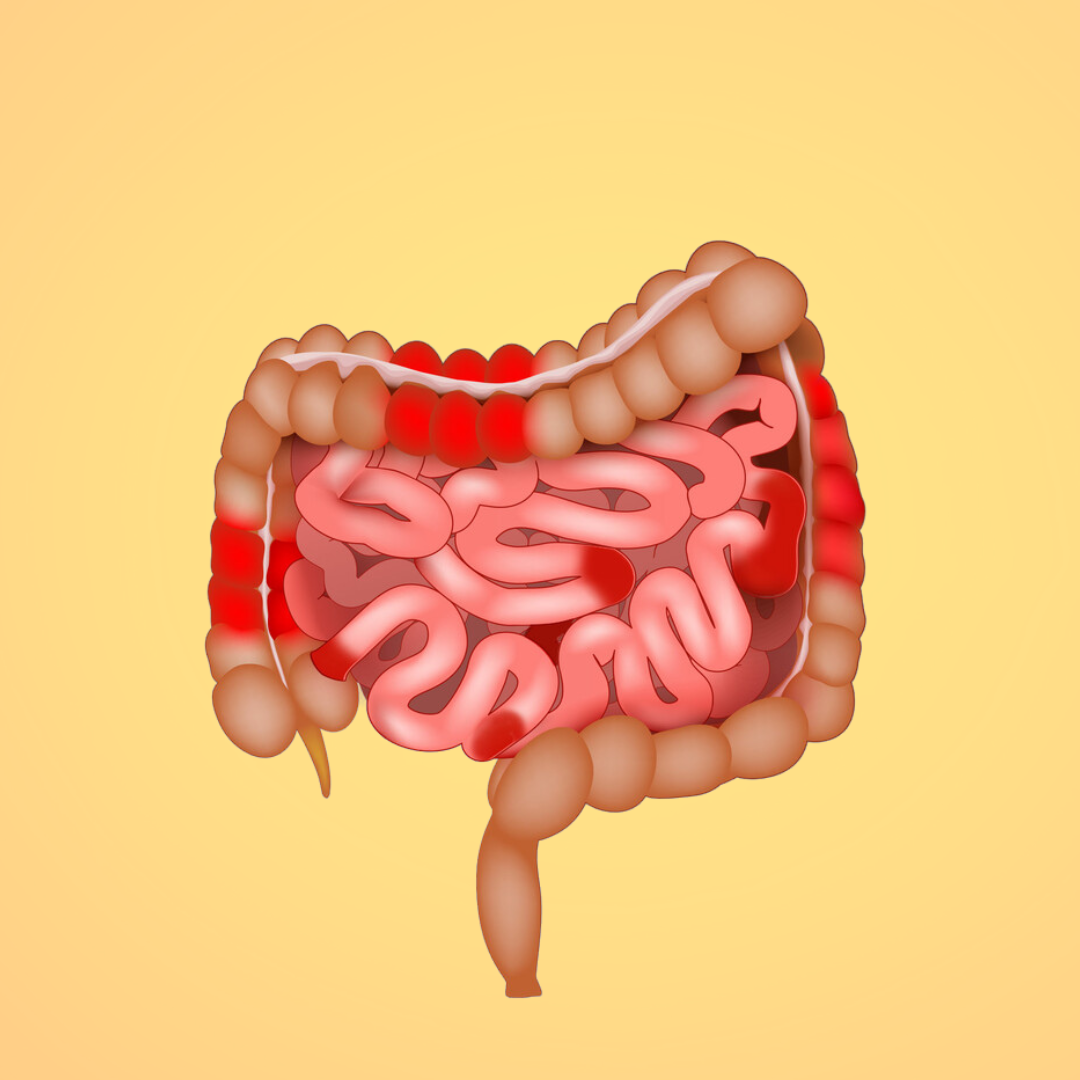
Irritable Bowel Syndrome (IBS) and Crohn's Disease are two distinct gastrointestinal conditions that can present with similar symptoms, often leading to confusion amongst patients and challenging diagnostic processes for healthcare providers. Whilst both conditions affect the digestive system, they have fundamental differences in their nature, diagnosis, treatment approaches, and long-term implications for patients' health.
Understanding the Basics
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder that affects the large intestine. Unlike structural or biochemical disorders, IBS doesn't cause changes to gut tissue that can be observed during medical examinations (2). Instead, it affects how the digestive system works, leading to various uncomfortable symptoms that can significantly impact quality of life (1).
Crohn's Disease, conversely, is an inflammatory bowel disease (IBD) that can affect any part of the digestive tract, from mouth to anus (5). It is characterised by inflammation that penetrates deep into the layers of bowel tissue, causing structural changes that can be observed through various diagnostic techniques (5).
Key Differences
The most significant distinction between these conditions lies in their inflammatory nature. According to Dolinger et al. (2024), Crohn's Disease causes visible inflammation and damage to the digestive tract, which can be observed through endoscopy and imaging studies (6). This inflammation can lead to complications such as strictures, fistulas, and abscesses (6). IBS, however, does not cause inflammation or tissue damage. Despite the discomfort and distress it causes, IBS doesn't lead to permanent changes in bowel tissue or increase the risk of colorectal cancer.
The diagnostic journey for these conditions differs substantially. Diagnosing Crohn's Disease typically involves a comprehensive array of tests, including blood tests to check for inflammation markers, stool samples to rule out infections and check for inflammation, various imaging studies such as MRI and CT scans, and endoscopy with biopsy (6). Some patients may also undergo capsule endoscopy for a more detailed view of the small intestine.
In contrast, IBS diagnosis relies primarily on symptom-based criteria, specifically the Rome IV criteria (7), and the exclusion of other conditions. Physical tests are limited and mainly serve to rule out other disorders. Healthcare providers heavily rely on patient history and symptom diaries to make an accurate diagnosis.
Symptoms and Manifestations
The symptom profiles of these conditions share some commonalities but have distinct characteristics. IBS typically presents with abdominal pain or cramping, bloating, and changes in bowel habits that may alternate between diarrhoea and constipation (1). Patients often experience relief from pain after bowel movements and may notice mucus in their stools (1, 2). Notably, blood in stools is not typically associated with IBS, and symptoms frequently worsen during periods of stress.
Crohn's Disease manifests with more severe symptoms, including persistent diarrhoea, blood in stools, significant weight loss, fatigue, and fever (8). Patients often experience reduced appetite and may develop extra-intestinal manifestations such as joint pain, skin problems, and eye inflammation. The chronic inflammation associated with Crohn's Disease can lead to more serious complications over time.
Treatment Approaches
Treatment strategies for these conditions differ significantly due to their distinct underlying mechanisms. IBS management focuses on symptom control and lifestyle modifications (3). Treatment typically begins with dietary adjustments, often including the low-FODMAP diet, which helps identify and eliminate trigger foods (3, 4). Stress management techniques play a crucial role, as psychological factors can significantly influence symptom severity. Other management strategies might include regular exercise, antispasmodic medications, and in some cases, antidepressants. Many patients also benefit from cognitive behavioural therapy and gut-directed hypnotherapy.
Crohn's Disease treatment aims to reduce inflammation and prevent complications. The treatment arsenal includes anti-inflammatory medications, particularly corticosteroids, along with immunosuppressants and biological therapies (8). Some patients may require antibiotics, especially when complications arise. In severe cases, surgery might be necessary to remove damaged portions of the digestive tract (8). Nutritional support is often essential, and regular monitoring is crucial to prevent and manage complications.
Long-term Outlook and Monitoring
The long-term prognosis for these conditions varies significantly. IBS, while chronic, typically doesn't worsen over time (2). Although it can significantly impact quality of life, it doesn't increase mortality risk or lead to serious complications. Many patients find that their symptoms improve over time with proper management and lifestyle adjustments.
Crohn's Disease, being a progressive condition, requires vigilant monitoring and ongoing management. The condition can lead to serious complications if not properly controlled, and many patients may require surgery at some point in their lives. There's also an increased risk of colorectal cancer, necessitating regular screening (9). However, the disease often follows a pattern of remission and flare-ups, and modern treatments can help many patients achieve and maintain remission.
The Role of Diet and Lifestyle
Both conditions benefit from careful attention to diet and lifestyle, though specific approaches differ. For IBS, dietary management often centres around identifying and avoiding trigger foods, maintaining regular meal patterns, ensuring adequate fluid intake, and managing stress levels (4). The low-FODMAP diet has shown particular promise in managing IBS symptoms, though it requires careful implementation and monitoring.
For Crohn's Disease, dietary management becomes more complex during flares, often requiring a low-residue diet (10). Proper nutrition is crucial, with particular attention paid to protein intake and supplementation of essential nutrients like calcium and vitamin D. Patients often find success with eating multiple small meals throughout the day and maintaining proper hydration.
Conclusion
While IBS and Crohn's Disease may initially present with similar symptoms, they are fundamentally different conditions requiring distinct approaches to diagnosis and treatment. Understanding these differences is crucial for healthcare providers and patients alike, as it influences treatment decisions and long-term management strategies. The key distinction lies in the inflammatory nature of Crohn's Disease versus the functional nature of IBS, driving varying approaches to diagnosis, treatment, and long-term monitoring.
For individuals experiencing persistent gastrointestinal symptoms, seeking proper medical evaluation is essential for accurate diagnosis and appropriate treatment. The growing understanding of these conditions continues to improve our ability to manage them effectively, offering hope for better outcomes for affected individuals. Through careful management and appropriate medical care, many patients with both conditions can achieve significant improvement in their symptoms and quality of life.
References
- Saha L. (2014). Irritable bowel syndrome: pathogenesis, diagnosis, treatment, and evidence-based medicine. World journal of gastroenterology, 20(22), 6759–6773.
- Cleveland Clinic. (2024). Irritable Bowel Syndrome (IBS).
- Anastasi, J. K., Capili, B., & Chang, M. (2013). Managing irritable bowel syndrome. The American journal of nursing, 113(7), 42–53.
- Jayasinghe, M., Karunanayake, V., Mohtashim, A., Caldera, D., Mendis, P., Prathiraja, O., Rashidi, F., & Damianos, J. A. (2024). The Role of Diet in the Management of Irritable Bowel Syndrome: A Comprehensive Review. Cureus, 16(2), e54244.
- National Institute of Health. (2024). Definition & Facts for Crohn's Disease.
- Dolinger, M., Torres, J., & Vermeire, S. (2024). Crohn's disease. Lancet (London, England), 403(10432), 1177–1191.
- Lacy, B. E., & Patel, N. K. (2017). Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. Journal of clinical medicine, 6(11), 99.
- NHS. (2024). Crohn's disease: Symptoms.
- Khatri, M. (2022, November 14). Crohn's and Colon Cancer: What's the Link? Web MD.
- Caio, G., Lungaro, L., Caputo, F., Zoli, E., Giancola, F., Chiarioni, G., De Giorgio, R., & Zoli, G. (2021). Nutritional Treatment in Crohn's Disease. Nutrients, 13(5), 1628.